Best of Johannesburg
Why the NHI Bill Is Poised to Redefine Private Healthcare in SA in 2025

In May 2024 the National Health Insurance (NHI) Act became law. Its goal is simple but disruptive: one national fund paying for healthcare for all South Africans. For Joburg’s private hospitals, doctors, insurers, and patients, 2025 is already showing how the law is shifting the ground beneath the system.
The NHI promises greater equity, but it also introduces financial and operational hurdles that could change private healthcare forever.
What the Law Brings
The Act creates a single national fund to pay for essential health services. Private medical schemes will no longer be allowed to cover anything that the NHI already funds. Their future role will be limited to supplementary cover for services excluded from the state package.
For private providers the rules are equally clear. Hospitals and specialists must be accredited by the Office of Health Standards Compliance if they want to work with the Fund. Services covered by NHI will be reimbursed at fixed rates set by the Fund, not at prices decided by providers themselves.
This effectively pulls private hospitals into the public funding framework, even as they remain privately owned.
Impact on Joburg’s Private Sector
Changing Patient Base
Hospitals in Johannesburg, which have historically relied on wealthier patients with medical aid, are preparing for a very different patient mix. More people who once depended on public clinics could now seek treatment at accredited private hospitals. That means higher patient volumes but lower income per case, as fees are capped by the Fund.
To keep an edge, many hospitals are already considering a stronger focus on elective and specialist treatments that fall outside NHI coverage. These could range from certain surgeries to advanced therapies that are unlikely to be fully subsidised.
Revenue and Contracting
Private hospitals and doctors have long enjoyed faster payments from medical schemes and self-paying patients. Under NHI they will depend on reimbursements from a national fund. That raises the risk of payment delays and cash flow pressures.
Medical schemes, meanwhile, are bracing for a drop in membership. Many South Africans may decide it no longer makes sense to pay for comprehensive cover when NHI provides the basics. For schemes, the future will be about reinventing themselves around supplementary benefits.
What It Means for Medical Schemes
Medical schemes are at a crossroads. Their traditional model of offering full cover is being dismantled. From now on, their role will be to fill the gaps, providing insurance for services that the NHI does not include.
That could mean smaller risk pools, fewer members, and less revenue. Administrators will need to rethink their products, possibly focusing on niche services or premium elective cover. Tax credits that once cushioned members are also expected to fall away, further shrinking their appeal.
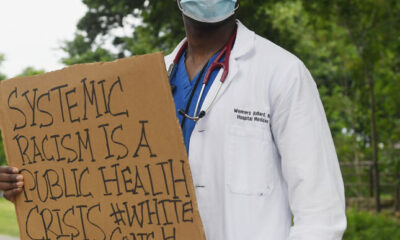
What People Are Saying
South Africans are divided. On one side are those who welcome the chance to walk into a private hospital without needing a medical aid card. For many Joburg residents who struggled with the public system, that feels like overdue fairness.
On the other side are those concerned about quality, waiting times, and whether the state can realistically manage such a vast fund. Healthcare professionals worry about losing autonomy and the possibility of a brain drain if compensation is squeezed too tightly.
Adding to the uncertainty are court challenges from professional associations and medical scheme bodies, arguing the Act contains constitutional flaws and an unclear funding model.
Risks and Opportunities
There are undeniable risks:
-
financial sustainability of the Fund is still unproven
-
corruption and mismanagement remain concerns
-
clarity on which services will be covered is still missing
-
rollout timelines stretch well into the future, leaving a long transition period
But there are also opportunities. Done well, the NHI could reduce inequality, improve access, and bring more patients into the doors of private hospitals that might otherwise have stood empty.
Johannesburg as a Testing Ground
Joburg’s private healthcare sector is uniquely placed to set the tone. With some of the country’s best-equipped hospitals and the largest concentration of scheme members, the city will likely be the first to feel both the benefits and the pain points of NHI implementation.
Hospitals that move early to secure accreditation, streamline costs, and diversify services could become models for the rest of the country. Medical schemes that pivot quickly to clear, affordable supplementary products may still hold onto loyal members.
The NHI is no longer just policy on paper. It is already reshaping how South Africa thinks about private healthcare. For Joburg patients it promises broader access. For hospitals and schemes, it demands reinvention. The city’s healthcare sector is in transition, and how it adapts now will define its future.
Also read: Retirement Age in South Africa 2025: What’s Actually Changing and What’s Not
Follow Joburg ETC on Facebook, Twitter, TikT
For more News in Johannesburg, visit joburgetc.com
Featured Image: Latitude Consultancy